Create your first automation in just a few minutes.Try Studio Web →
UiPath QPP Participation Check for Healthcare
by YouTube
0
Activity
<100
Summary
Summary
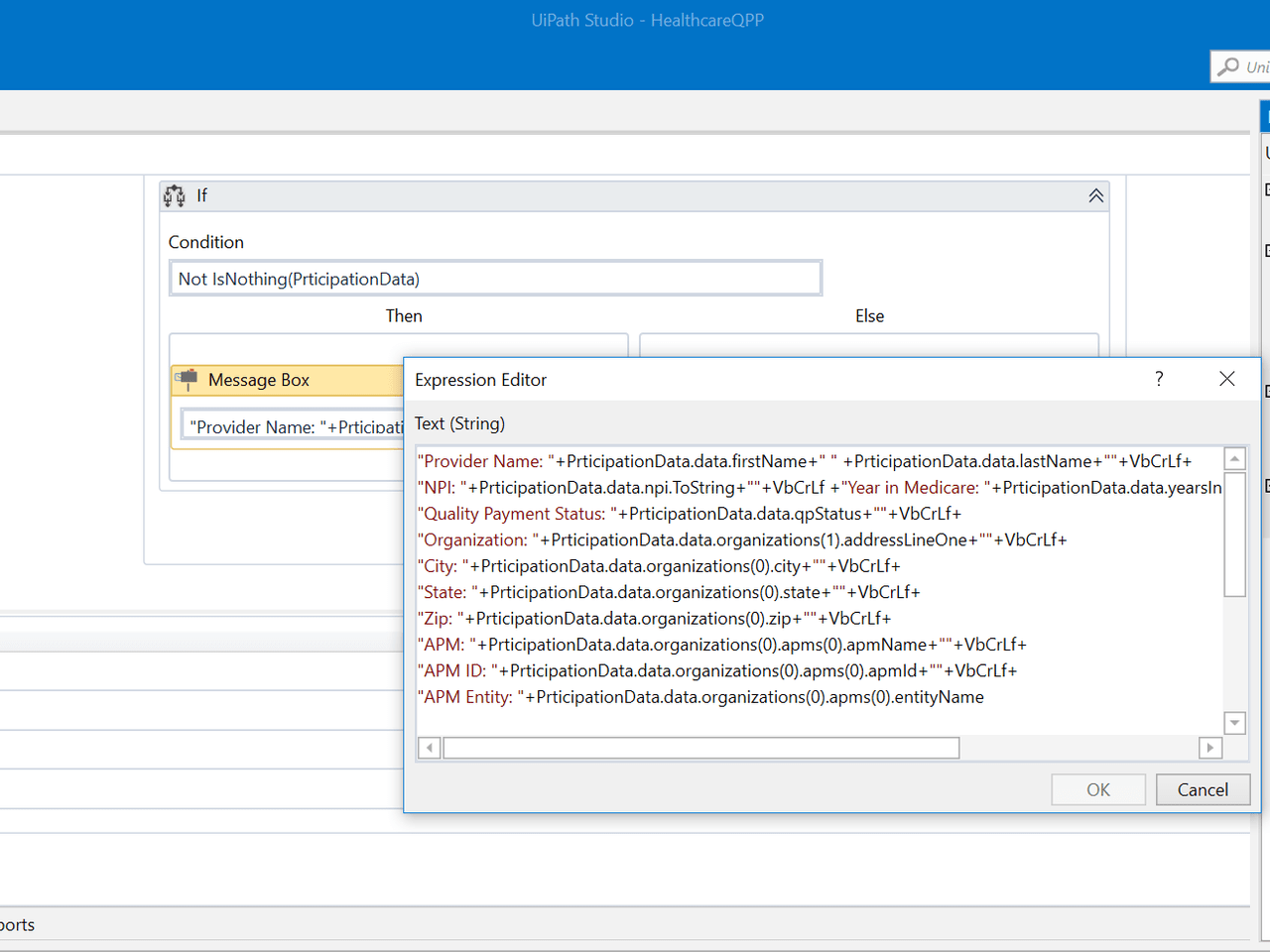
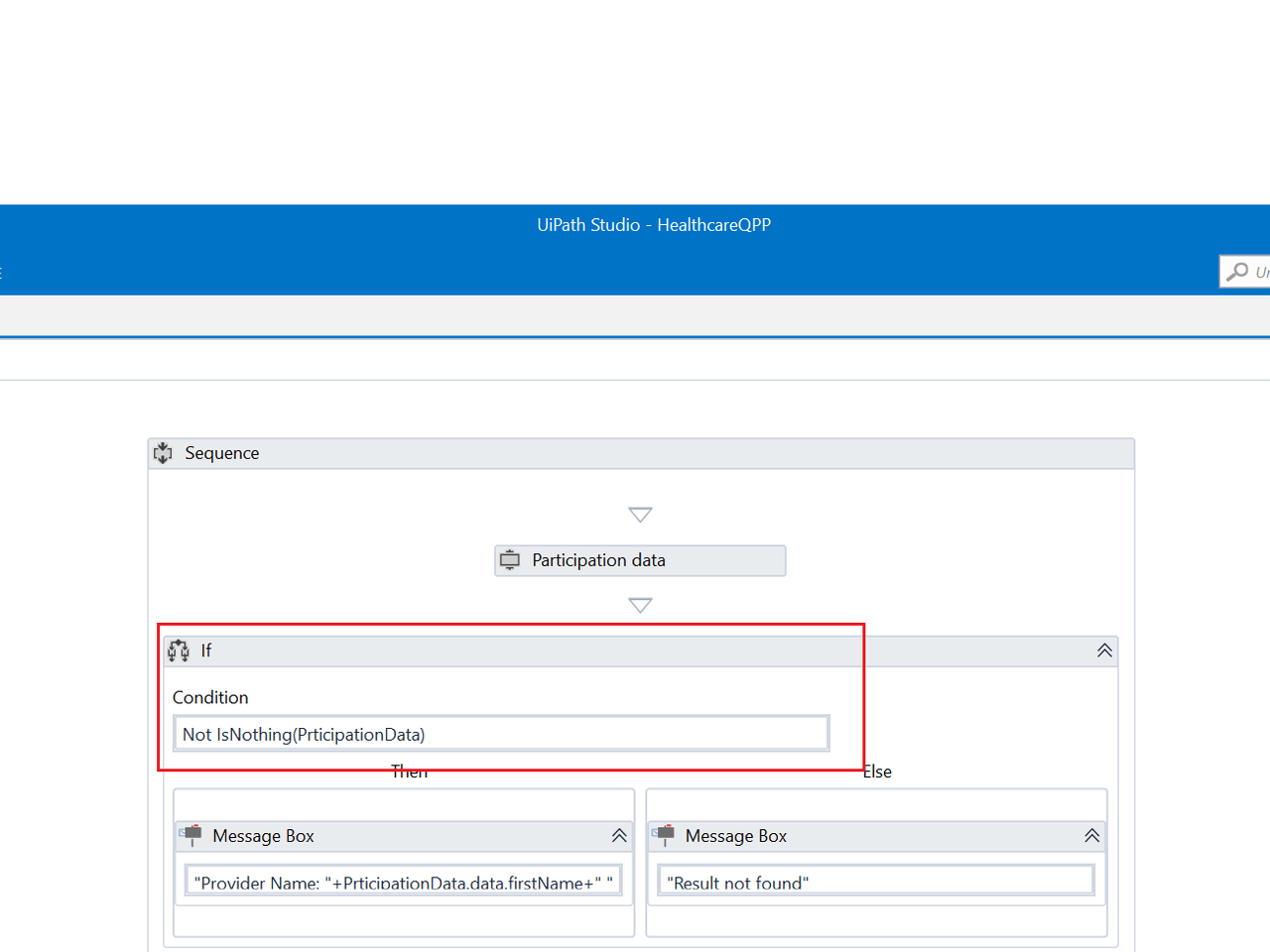
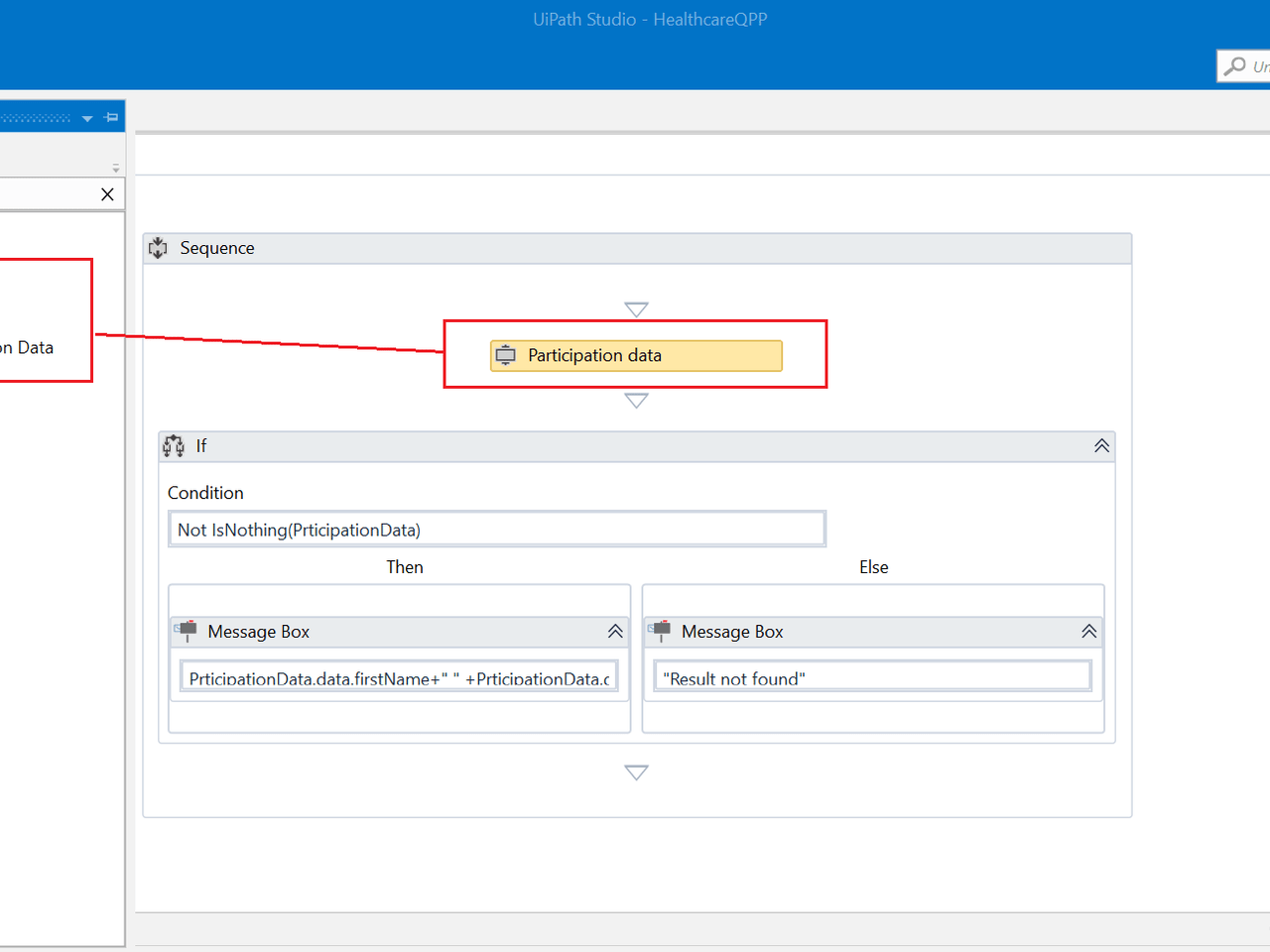
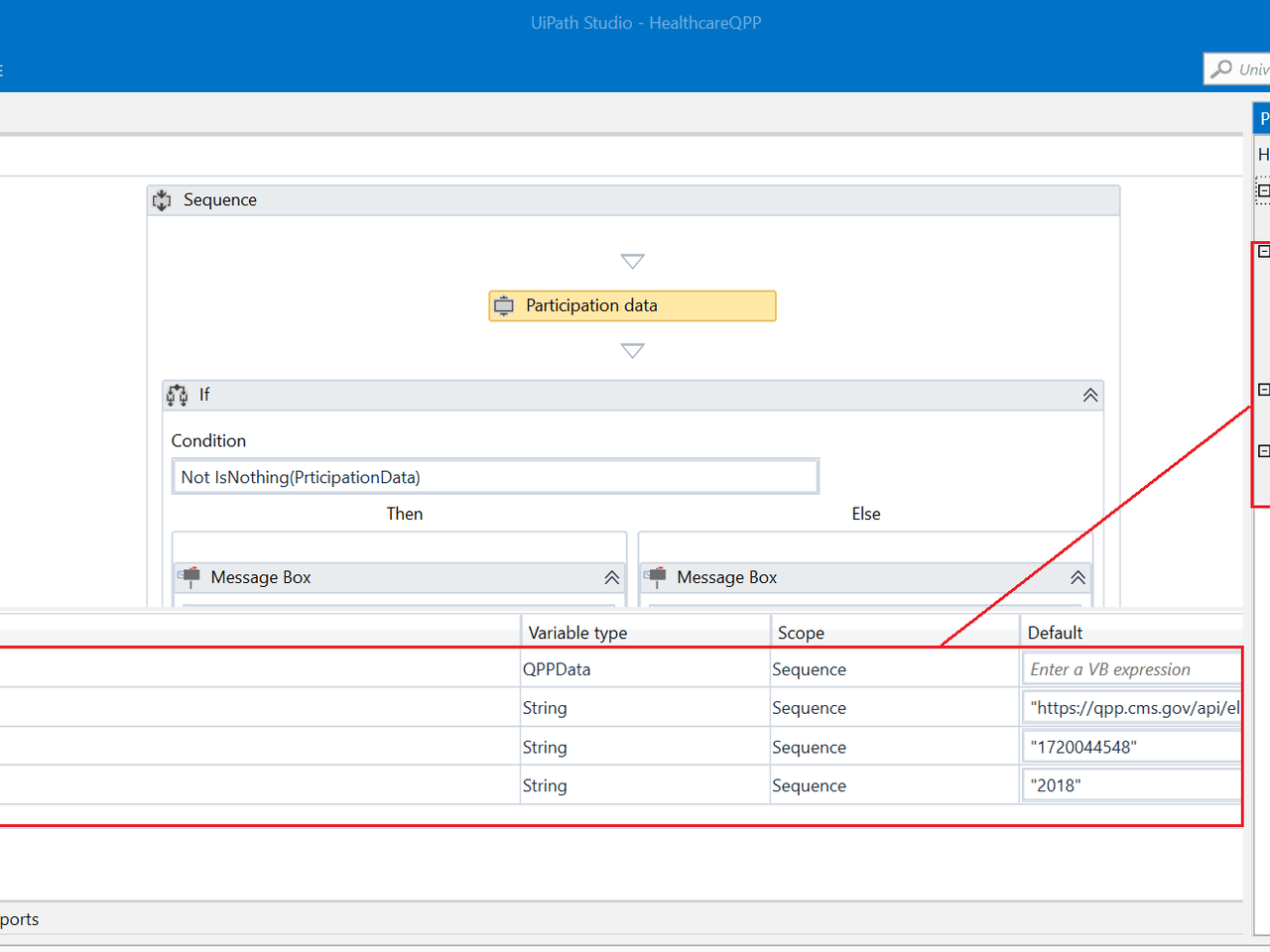
UiPath Accelerator for real time Provider lookup for Quality Payment Plan participation through the API provided by CMS and bring provider's QPP participation details for validation & processing
Overview
Overview
As per the guidelines from Centers for Medicare and Medicaid Services (CMS), all eligible providers are required to participate in the Quality Payment Program (QPP) or face financial reimbursement penalty.
CMS will establish a performance threshold for the composite score for each year. Clinicians who score above the threshold earn bonuses; those who score below it face penalties. Bonus and penalty amounts align with the scores (e.g., the higher the score, the greater the bonus).
QPP performance is measured for each calendar year, with payment adjustments disbursed two years later (i.e., 2017 performance will determine 2019 adjustments). Between 2017 and 2019, the increase to the base Medicare physician fee schedule is 0.5% annually. Between 2020 and 2025, the base Medicare physician fee schedule will be held constant (0% increase); adjustments to reimbursement during that time will come exclusively from payments made through the QPP. Starting in 2026, participants in the Merit-based Incentive Payment System (MIPS) will receive a 0.25% annual increase in the base rate; participants in Advanced Alternative Payment Models (Advanced APMs) will receive a 0.75% annual increase in the base rate, in addition to performance-based payment adjustments through either MIPS or their APM.
This component will help to validate the Provider Performance for Physicians Participating in the Merit-Based Incentive Payment System (MIPS) .
Features
Features
Validation of the provider if he/she is registered with CMS for QPP This validation accelerator can be utilized as per the business process requirement for processes such as Provider Quality Payment participation check, validation of different organization, validation of Bonus and penalty based on provider participation.
Additional Information
Additional Information
Dependencies
Newtonsoft.Json >=10.0.3
Code Language
Visual Basic
Runtime
Windows Legacy (.Net Framework 4.6.1)
Technical
Version
1.0.0Updated
February 18, 2020Works with
UiPath Studio 2018.3+
Certification
Silver Certified
Tags
Support
UiPath Community Support
Resources