Create your first automation in just a few minutes.Try Studio Web →
UiPath Provider Credentialing for Healthcare
by YouTube
0
Solution
<100
Summary
Summary
Healthcare provider credentialing process is a pillar of quality and risk management for the healthcare industry, it’s critical for facilities to perform their due diligence for provider onboarding
Overview
Overview
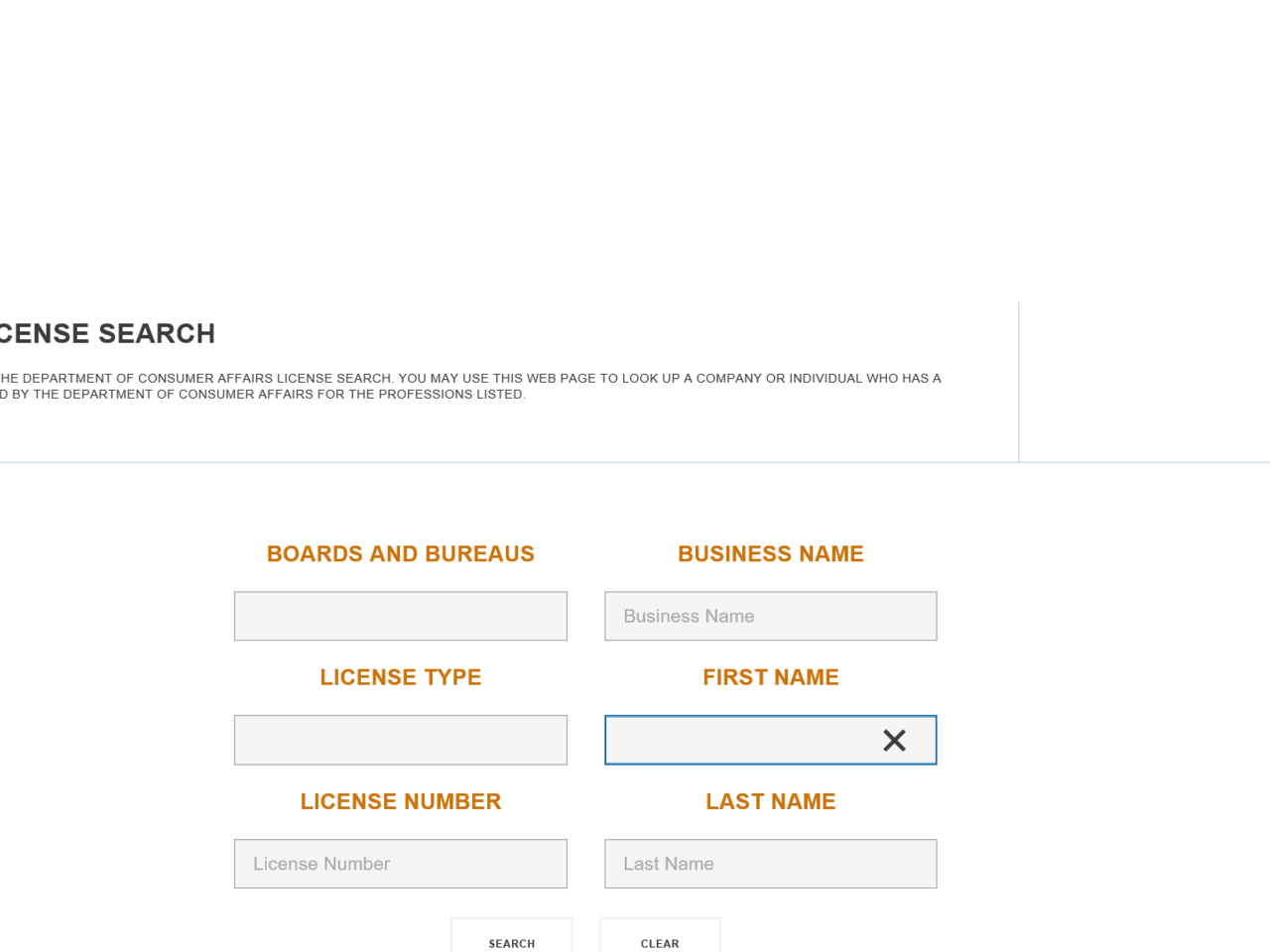
Provider Credentialing is an essential process that both Payers and Providers manage to ensure their clinical staff is qualified and certified to practice in their network . The healthcare provider credentialing process is a pillar of quality and risk management for the healthcare industry, it’s critical for health facilities to perform their due diligence when hiring/appointing front-line medical services providers. Credentialing is the process to verifies that a physician has the necessary education, experience, training, licensure, history, and competencies to perform specified medical procedures.
Credentialing process is required during the hiring/ appointing process and at other intervals afterward, this process follow practices established by regulatory and accreditation organizations such as the Joint Commission. Below is the list of main steps of verification in credentialing process
Board Certification – Verify current certificate level
Sanction Check– Verify OIG sanction check
Department of Health and Human Services
DEA certification/registration
Work History – extract work history from the curriculum vitae
NPI Validation – query state license and Medicaid/Medicare
Features
Features
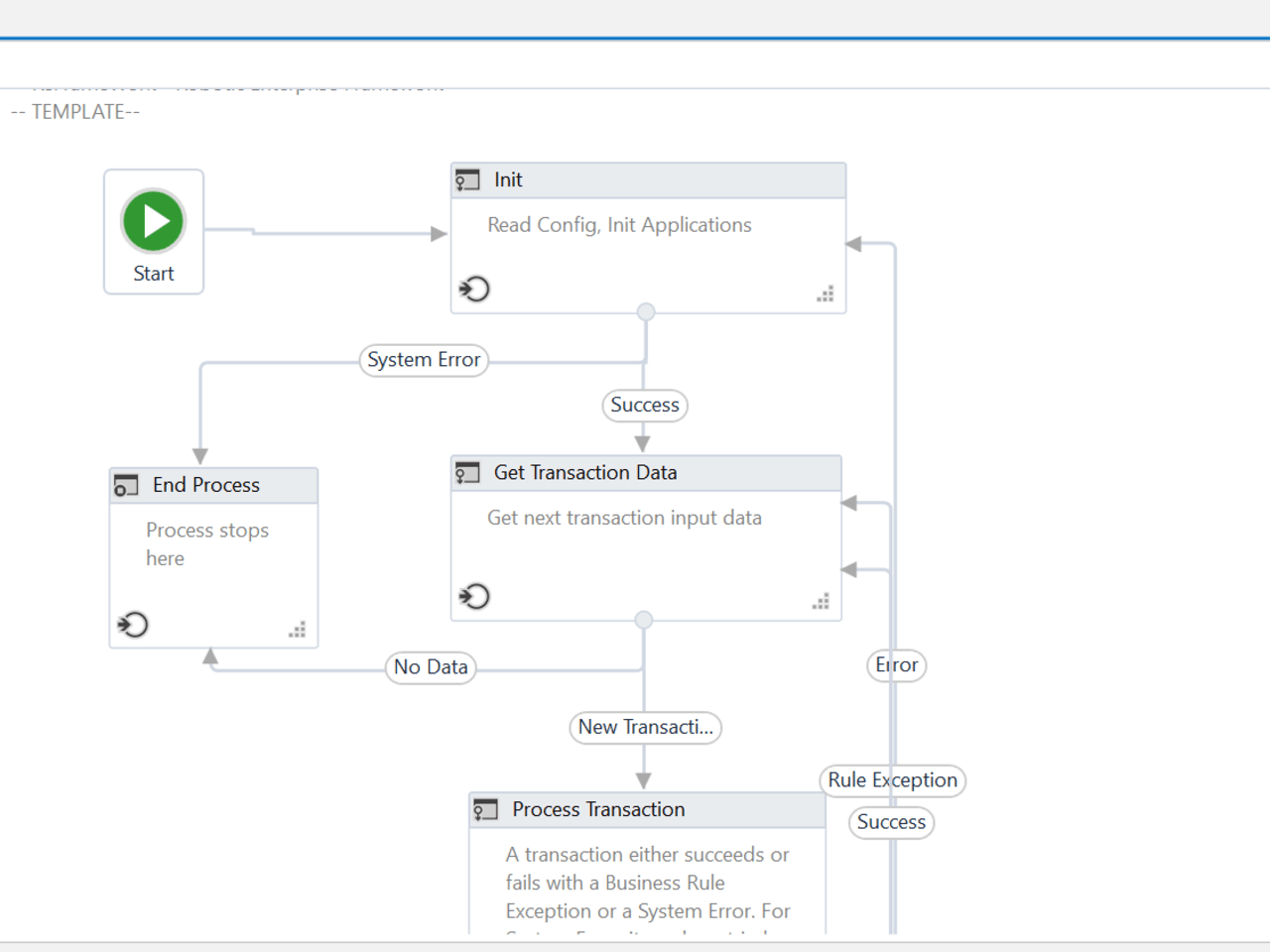
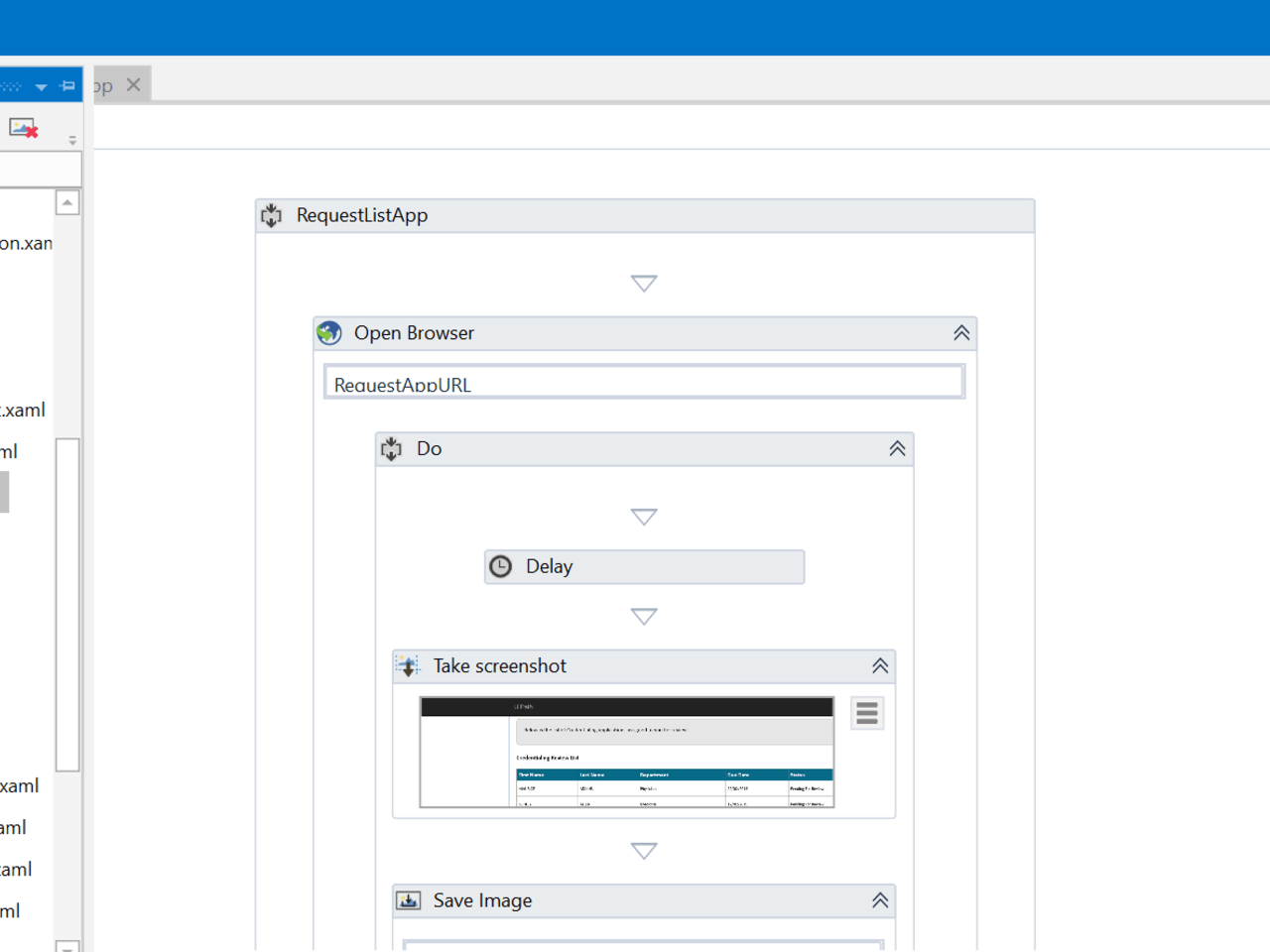
Automation will Increase the efficiency of a workflow by improving the coordination of the activities, it will bring below listed benefits Improved Productivity –An automated and streamlined Provider Credentialing process results in increased team productivity with reduction in processing errors Reduced operating costs – Reduction in manual primary source verification, sanction check & license verification results in increased process efficiency and reduced operation cost Enhanced Provider Experience – Automated process will decrease the provider onboarding time and involvement and enables the payers to maintain enhanced collaboration levels and reduce turnaround time Improved compliance – The ability to retain and audit at any point in the process allows for better recordkeeping
Additional Information
Additional Information
Dependencies
Newtonsoft.Json >=10.0.3 Healthcare Provider NPI Search Activity Healthcare Provider Sanction Validation Accelerator
Technical
Updated
February 19, 2020Works with
UiPath Studio 2018.3+
Tags
Support
UiPath Community Support